ACA requirement saves women money
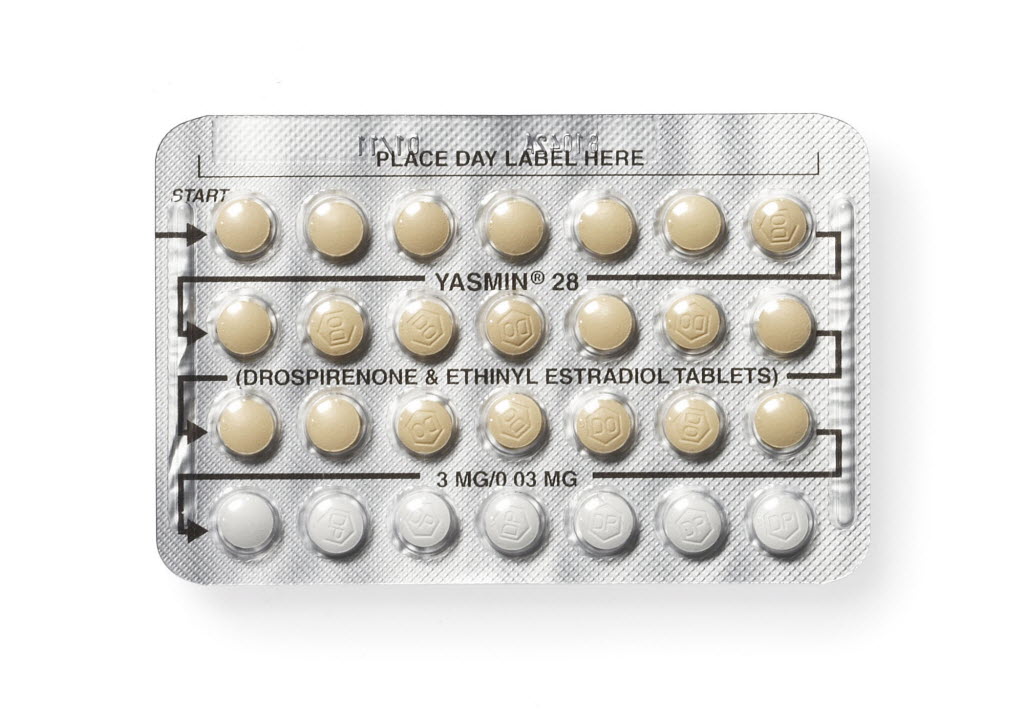
Women saved hundreds of dollars in the first year after the Affordable Care Act required insurers to cover prescription contraceptives.
The health law required the coverage of most forms of prescription birth control without additional out-of-pocket costs. The amount women saved and the speed with which they realized those savings surprised researchers, according to the Kaiser Family Foundation.
The study found that the average birth control pill user saved $255 the year after the requirement took effective, and the average user of an intrauterine device (IUD) saved $248.
“These are healthy women and this on average is their No. 1 need from the health care system,” said Nora Becker, lead author of the study, in the Kaiser article. “On average, these women were spending about 30 to 44 percent of their total out of pocket (health) spending just on birth control.”
For more plans, the requirement began Aug. 1, 2012 or Jan. 1, 2013. Some grandfathered plans are exempt from the mandate, as are some religious-based plans.
Researchers question whether the new requirements will lead to a shift to longer acting methods of birth control.
“If prior to the ACA a woman was facing $10 to $30 a month for the pill but hundreds of dollars upfront for an IUD and now both are free, we might see a different choice,” Becker said in the article.
While spending on most birth control dropped, it didn’t change much for the vaginal ring or hormonal patch. Researchers suspect that’s because under the original rules, many insurers declined to make the ring or patch free since they are essentially hormone delivery methods.
This year, however, the Obama administration made is clear that while insurers don’t have to cover every brand of every method, they do have to cover at least one product in each category.
